Healthcare technology integration may seem vague at first. After all, there are many healthcare organizations, care levels, and software that deal with patient information. Where to start? What to connect? We'll dismantle the concept into pieces that are easy to understand.
Key takeaways
- Healthcare integration aims to connect patient information siloed in different systems, improving efficiency, automating processes, and reducing costs. During the process, providers standardize data, ensure its correct interpretation, and enhance its secure storage and transmission.
- The major challenges that go along with the unification process include a lack of data standards for secure records storage and interchange, security risks, intricate regulatory compliance, legacy systems, and a shortage of resources for change.
- Medical integration can take various forms, ranging from vertical models that connect different levels of care to horizontal models that unite the same levels of care, as well as more advanced, technology-based integrations and those that focus on care coordination.
- NEKLO experts can help to align disparate data sets, enabling systems to talk to each other in one language, eliminating misinterpretations. We build and integrate healthcare software so that you enjoy long-term benefits and your patients receive quality, tailored care.
What is healthcare technology integration, and why does it matter
Healthcare technology integration involves connecting disparate devices, software, systems, and services to facilitate secure data exchange. While integration can take different sizes and forms, the core remains the same: data interoperability.
At the dawn of the data connectivity era, most healthcare software was represented by standalone, on-premises systems. Soon, inefficiencies begin to accumulate, including duplicate records, delayed care coordination, and compliance risks. At this point, it was obvious that the fundamental shift towards integrated healthcare systems was inevitable.
Linking siloed data between hospitals, clinics, and departments improves operational efficiency, care quality, and patient outcomes. Nevertheless, achieving data interoperability can be challenging, and there is no one-size-fits-all solution. The critical factors include location (country, state), participation in healthcare alliances, organizations' size, level of care, and specialty.
How geographical position within the US impacts healthcare data integration
Core facts and statistics
In 2025, healthcare software integration remains a consistent trend globally. According to Grand View Research, the world's healthcare data integration market size was assessed at $1.05 billion in 2022 and is slated to climb to $3.11 billion by 2030, reflecting a compound annual growth rate of 14.5% from 2023 to 2030.
What does it mean for healthcare providers? More efforts and investments in software interoperability to cut costs, optimize processes, and deliver quality care. McKinsey estimates that combinations like EHR+e-prescriptions (or other tools) can increase the healthcare system efficiency by 15% on average.
Real results of such changes include:
- fewer readmissions
- annual budget savings
- medication error reductions
- more informed, timely clinical decisions
- patient outcomes improvement
- saved staff time that can be dedicated to care, and more.
The major factors contributing to the growth of the medical integration market include the increasing volume of data generated by the healthcare system, the need to enhance efficacy, rising healthcare costs, and the demand for improved patient safety.
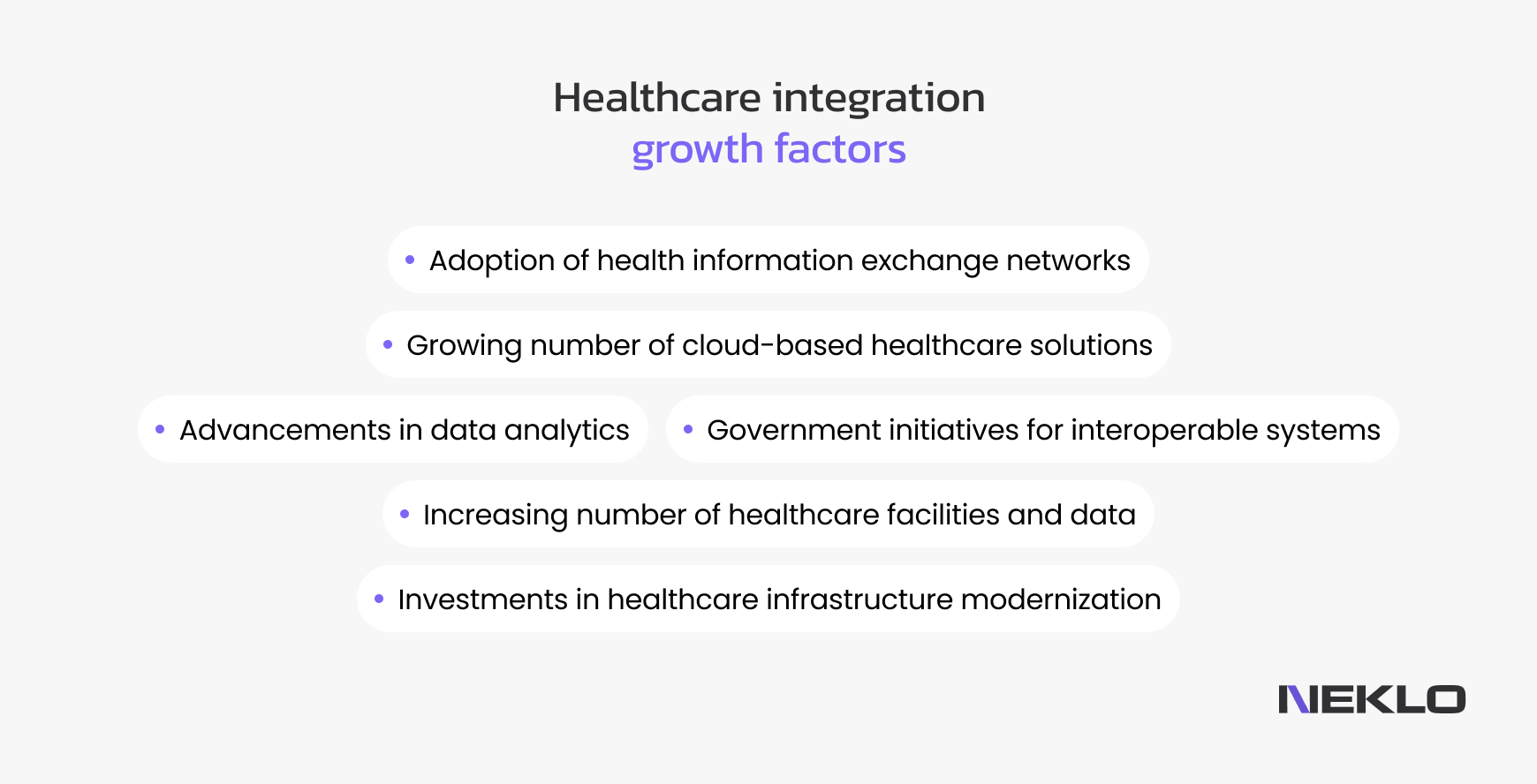
Moreover, the expanding global adoption of clinical and non-clinical healthcare IT integration, wider acceptance of patient monitoring, and better access to telehealth also drive the market forward. A consistent rise in EHR use evokes the need for its integration with radiology and lab systems.
Large enterprises, such as multi-hospital systems, nationwide provider networks, or large insurance/payor companies, are the major adopters of healthcare integrated solutions. They can afford wide-scale changes, have more complex data integration requirements, and require fast scaling of operations.
SMEs are projected to show the fastest CAGR in the period 2022–2030 due to the adoption of cloud-based data integration solutions, the need to enhance efficiency while cutting costs, increasing compliance requirements, and minimizing manual tasks.
- North America remains the dominant region, with a 38% market share, while the Asia Pacific is considered a promising region for healthcare integration advancements.
Hospitals are major adopters of data integration initiatives. GlobeNewswire states that they account for 72.3% of the IT healthcare integration market share. Clinics and laboratories are also expected to advance, as the volume and data complexity steadily increase. Other end-users include ambulatory care centers, research institutions, academic medical centers, and public health networks.
Benefits of integrated medical solutions
The advantages of medical data connection affect not only hospitals and clinics but also all healthcare participants, including patients, research teams, and health insurers.
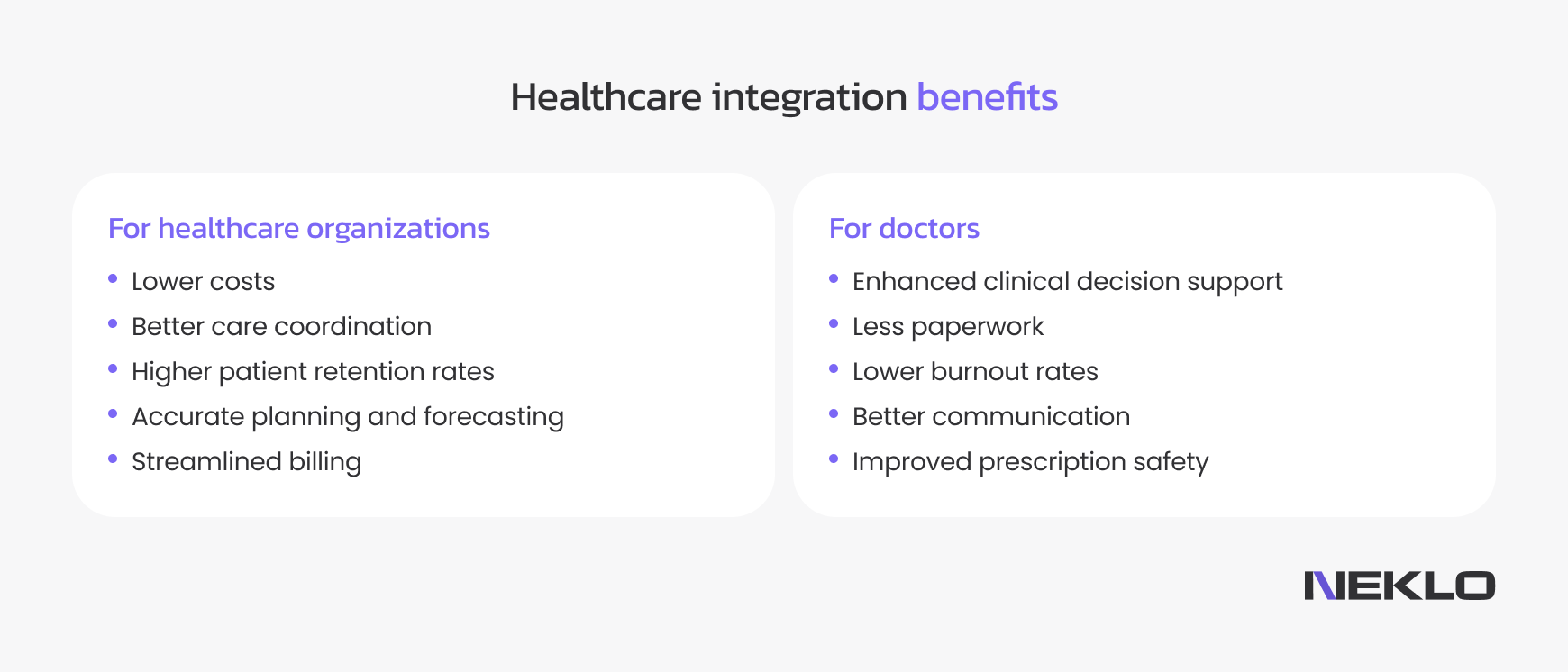
For healthcare organizations
Integrated healthcare improves operations for hospitals, clinics, and private practices. It cuts the time doctors spend on filling out documents by automating workflows and data entry. The result is fewer errors in diagnosis, billing, scheduling, and claims processing.
Other benefits include:
- Lower IT costs: integrated healthcare systems eliminate duplicate systems and legacy software maintenance spending, meaning more money can be spent on patient care.
- Improved care coordination: interoperable software enables data sharing between facilities, specialties, and professionals that allows different professionals to access data in real time, reducing care delays and test duplications.
- Better patient retention: organizations that leverage interoperability have stronger brands in a competitive market. Shorter patient wait times, better diagnoses, and consistent treatment across providers are just a few of the benefits patients receive from integrated care.
- Accurate planning and forecasting: connected systems enable real-time hospital occupancy monitoring, better analytics, and precise predictions on patient demand and staffing levels.
- Streamlined billing and claims management: while disparate systems spawn delays in claim processing, errors from manual input, and higher rejection rates, automation and smooth data flow improve patient experience and cause no revenue delays for the business.
Example: Epic + Cerner + PACS integration for a hospital network.
For doctors
With integrated healthcare solutions, healthcare professionals get a single patient view across multiple facilities. As a result, doctors and clinicians have less paperwork, lower burnout rates, and enhanced clinical decision support, leading to more accurate diagnoses and improved patient outcomes.
More advantages for healthcare professionals include:
- Improved prescription safety: no more missing drug-to-drug, drug-to-allergy, and drug-to-condition interactions or duplicate prescriptions that may disrupt care.
- Fewer duplicate tests and prescription errors: syncing across connected providers helps to avoid repeated and costly tests and procedures, as well as delays in care delivery.
- Better communication: critical updates like test results, diagnoses, and discharge summaries reach other providers quickly. It leads to decreased readmission rates and helps different professionals develop unified personalized care plans.
Example: a cardiologist accesses imaging, lab, and vitals data in one dashboard.
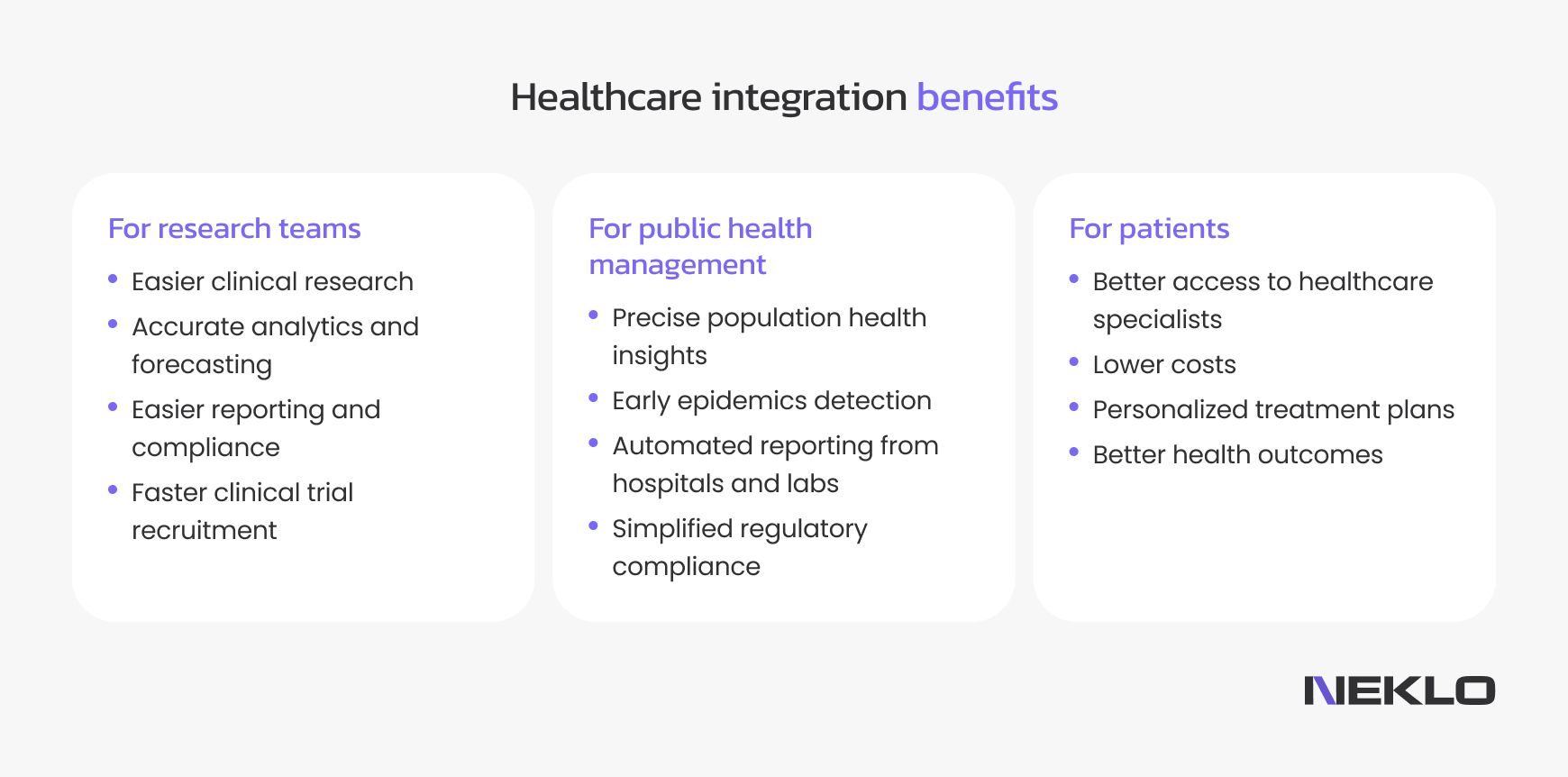
For research teams
Integrated medical solutions facilitate clinical research, drug discovery, quality reporting, and compliance for research teams. Connected and standardized data from imaging, IoT devices, and genomics databases helps to explore complete patient journeys, enabling more accurate findings.
Other perks include:
- Real-time access to multi-site datasets: data collection from diverse populations leads to more inclusive and comprehensive studies.
- Faster clinical trial recruitment: researchers can easily find patients for clinical trials, leading to quicker recruitment, higher enrollment figures, and shorter trial timelines.
- Easier FDA reporting and compliance: researchers avoid costly delays and simplify FDA submissions and approval timelines through traceable logs of trial data handling, harmonized data for cross-border studies, and integrated eConsent platforms.
- Predictive models development: accurate analytics and forecasting help mark people at high risk of illness and introduce a proactive approach to treatment.
Example: Genomics + EHR integration for precision medicine.
For public health management
Healthcare integration helps to gain centralized population health insights and discover the health needs of specific populations. It also makes it easier for the authorities to access top-tier compiled information for shaping public strategies and more cost-efficient ways to guarantee adherence.
More benefits include:
- Early detection of outbreaks and epidemics: real-time data shows the rise of disease levels in particular areas, helping to deploy preventive measures in a timely manner.
- Automated reporting from hospitals and labs: organizations connect their systems via secure protocols like FHIR / HL7, DICOM, and IHE, delivering normalized, de-duplicated data to local, state, and federal health authorities.
- Simplifies compliance with TEFCA, HIPAA, and GDPR: data unification enhances compliance by automating security, consent management, and audit tracking. Only necessary data is sent to public health agencies.
Example: Integrating EHR feeds into the Centers for Disease Control and Prevention
For patients
The global trend for patient-centered healthcare services continues to glow. It turned out to be more convenient than traditional models — no siloed information naturally leads to more connected and personalized care. Telemedicine, pharmacy, and lab data unified in real time help patients to get help when they need it the most, detect disease at early stages, and get tailored treatment plans.
Among the other advantages are:
- Improved specialists availability: healthcare technology integration improves scheduling and reduces waiting times and no-shows. Patients can easily book an appointment and get a consultation remotely.
- Lower costs: with overall health history in front of the doctor, there are fewer unnecessary or duplicated lab tests — just increased efficiency, faster prescriptions, and optimized insurance approvals.
- Tailored treatment: precise diagnoses, therapies, and care plans become possible due to the combination of patient information from various sources, including lifestyle and behavioral data, EHR records, wearables, and predictive analytics.
- Better health outcomes: telemedicine, chronic disease monitoring, and wearables help track vitals, foresee health deterioration, promote timely doctor visits, and decrease hospital readmissions.
Example: Patients track glucose levels through integrated wearables + EHR.
Key components of a fully integrated healthcare system
- Electronic health records: integrated medical solutions provide error-free data interoperability, connecting EHR systems, labs, imaging, and pharmacy.
- Medical devices: medical device integration software securely transfers patient data in real-time for constant monitoring of patient health condition and their safety benefits.
- Healthcare integration software and APIs: middleware and data exchange standards like FHIR, as well as custom healthcare integration software, connect healthcare facilities and organizations, making data flow free of interpretation errors.
- Clinical decision support systems: these platforms provide clinicians with alerts, recommendations, and predictive insights. They should be increasingly integrated into EHR systems and telemedicine workflows to deliver accurate insights.
- Population health management platforms: they aggregate patient data from multiple sources and use analytics to identify risk groups and improve care plans. Such software facilitates value-based healthcare, which is a cornerstone of modern medical practice.
Types of healthcare integration models
Integration can take different forms depending on the organization's size, care model, and technological maturity. To build a fully connected healthcare ecosystem, providers combine organizational, service delivery, and technology-driven integration models.
Structural integration
Structural integration means connecting doctors and healthcare providers at one or different stages of care. The goal remains the same — to improve operational efficiency, drive better patient outcomes, and reduce costs. As the US healthcare system promotes provider integration and coordination, many models emerge in this sophisticated, multifaceted care delivery system.
.png)
Horizontal integration models
Horizontal integration happens when organizations at the same level of care merge or collaborate to improve efficiency, cut expenses, and unify operations. A single specialty group practice can connect its data to optimize workflows, or hospitals, labs, or imaging centers can form mergers or alliances between each other — hospitals with hospitals, labs with labs.
Integrated healthcare providers share infrastructure for IT, HR, and billing, and can initiate bulk purchasing and joint R&D investments, meaning shared data, costs, risks, and responsibility, as well as benefits. For example, the consolidation of EHR platforms between a group of regional hospitals leads to a reduction in licensing costs.
Vertical integration models
Vertical integration connects different levels of care under a single ecosystem, ensuring a continuous patient journey from preventive care to hospital treatment to home recovery. An integrated care delivery system combines primary care, specialist services, and inpatient care, aligns financial incentives between payers and providers, and improves care coordination and reduces duplication of services.
For example, a health insurance company can acquire a telehealth startup and several outpatient clinics to manage the entire patient lifecycle under one integrated framework. The same way hospitals can purchase medical equipment companies for a steady supply of required tools, removing the need to address third-party dealers.
Such models benefit all participants by diversifying revenue streams, achieving cost savings, increasing access to care, and improving quality and efficiency. On the other hand, they can be hard to manage and keep regulatory compliance, as different parts of the healthcare market are subject to various regulations.
Care coordination models
These integration types focus on aligning care delivery between hospitals, clinics, and specialists.
Integrated care delivery systems (IDNs)
An integrated delivery network or integrated care delivery system takes vertical integration further by creating a single governance structure that controls multiple facilities, providers, and care models.
One entity owns or manages hospitals, clinics, labs, pharmacies, and home care, delivering centralized decision-making and unified financial risk management. For example, a nationwide IDN connects 20 hospitals, 60 clinics, and a digital telehealth platform, enabling physicians to access patient records instantly across locations.
Patient-centered medical home (PCMH)
This model focuses on coordinated, team-based care where primary care providers act as the central hub for all patient health needs. It works as a single point of contact for the patient's entire journey, emphasizing preventive care, education, and ongoing monitoring.
A patient-centered medical home requires strong integration between EHRs, pharmacies, and specialists for a seamless data flow. For example, a clinic implements a PCMH model, using a healthcare integration platform to sync lab results, prescriptions, and clinical notes into one patient dashboard.
Outreach and technology-based integration
Another classification explains how technology brings together patients with clinics and hospitals via specialized platforms, apps, and devices.
Technology-led platform integration
Technology-led platform integration focuses on using technology as the primary means of integration to improve communication and access. It connects disparate healthcare systems, devices, and apps into one seamless ecosystem using APIs, middleware, and interoperability standards.
The adopters of this model use digital platforms, such as telehealth, electronic health records, care management software, and biomedical device integration, to link providers and patients. For example, a HealthTech startup can build a cloud-first integration layer that unifies wearables, lab systems, and telehealth into one platform, enabling real-time patient insights.
The key characteristics of this approach include:
- using FHIR, HL7, and custom API frameworks for data standardization
- integration of EHRs, IoMT devices, imaging systems, and analytics platforms for a 360-degree patient overview
- supporting predictive insights, population health management, and value-based care
- enabling faster innovation for startups and enterprise providers alike.
Mobile integrated healthcare (MIH)
Mobile integrated healthcare is a care model that brings medical services directly to patients at home or on-site. It often includes EMS teams, telehealth platforms, and connected monitoring devices.
As the name suggests, at the heart of mobile integrated health like mobile apps, IoMT wearables, and telehealth platforms. They integrate real-time patient data into provider systems like EHRs and patient portals, enabling timely care delivery for patients with disabilities that make it difficult to visit doctors offline and those who live in remote areas.
This model addresses gaps in traditional care by providing non-emergency services, particularly in chronic disease management and post-hospital follow-ups, thereby making healthcare services more accessible to diverse populations. For example, a medical team partners with a hospital's remote care platform to provide on-demand at-home care for chronic disease patients.
Challenges in healthcare integration
The demand for integrated healthcare has come together with the domain's digitalization. Smooth data exchange helps to deliver value-based, personalized care. Unfortunately, it's not that simple: there are as many rewards as complexities along the way. We'll unravel the main ones.
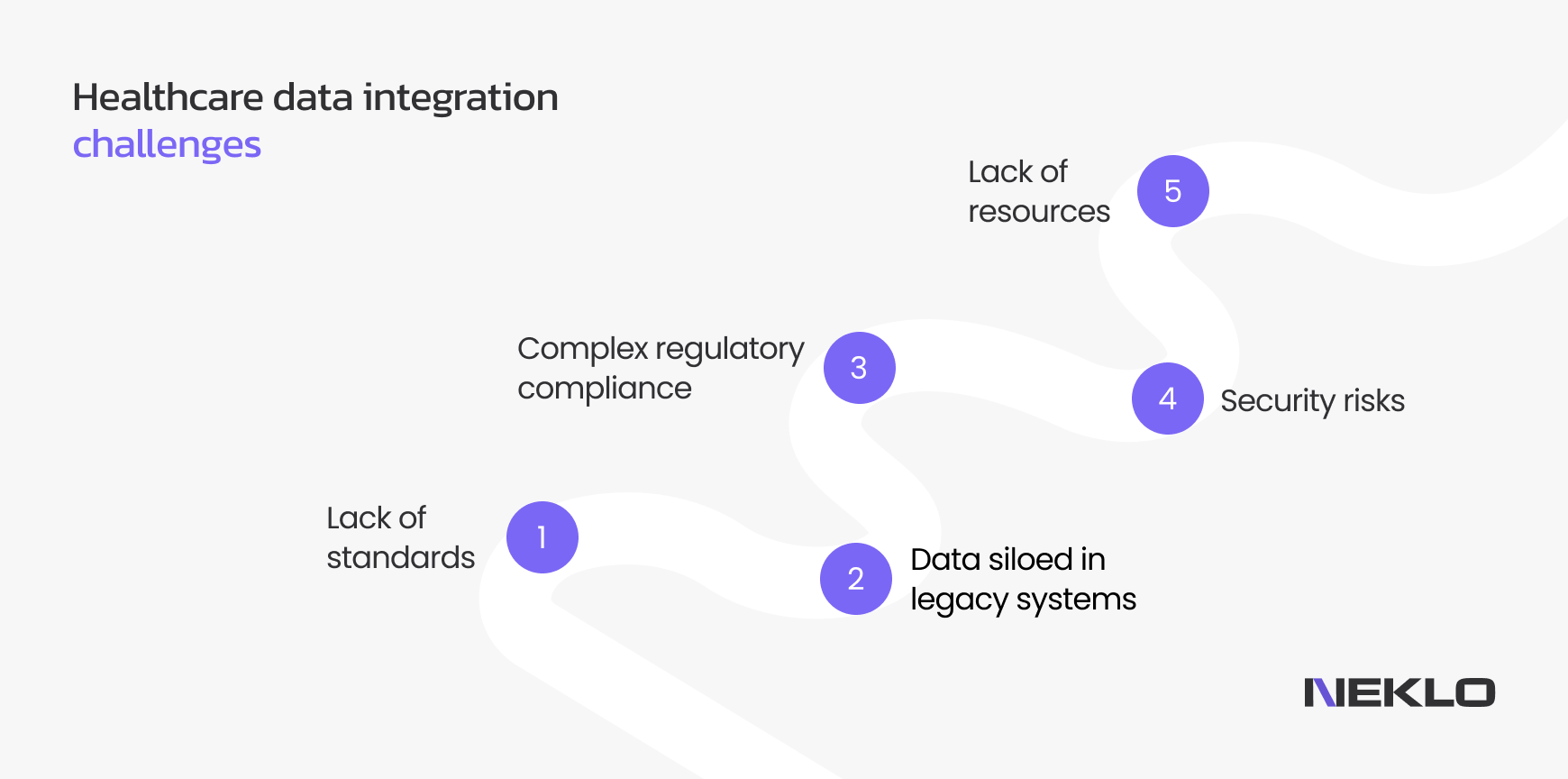
Lack of standards for data storage and interchange
Creation of integrated medical solutions and networks implies strict adherence to standards, and remains hard for healthcare organizations on their way to modernization. The research shows that 47% of healthcare leaders cite data quality and integration issues as major barriers to AI adoption, while 39% expressed concerns about regulatory compliance and data privacy.
Different data standards and communication protocols lead to their misinterpretation by other systems and errors while being transferred. Being a global issue, organizations handle the lack of standards by following the widely accepted interoperability protocols like HL7 and FHIR.
Legacy systems and infrastructure
As many healthcare organizations keep relying on outdated technology, it makes integration with newer systems difficult. They can be simply offline, like on-premises patient management systems, paper records, standalone imaging equipment, disconnected lab tools, etc.
How to face the challenge? First, you should run an assessment of the current solution, identify bottlenecks, prioritize upgrades, and evaluate costs associated with system maintenance. Then, you have several paths to follow: from encapsulation and refactoring to rebuilding or complete replacement. Develop a plan for gradual optimization aligned with your business goals and desired outcomes.
Compliance and regulations
A fragmented regulatory landscape within one country or across several countries significantly hampers healthcare software integration. The rules like HIPAA, HITECH, PIPEDA, GDPR, MDR, and ISO 13485 are country-specific, while regulations like IEC 62304 for medical software and ISO 27001 for information security are global. The problem is that integrated software must comply with every applicable framework simultaneously.
In addition, regulations are frequently changed, so you need to monitor these changes and adjust accordingly. If your integrations affect diagnostic, monitoring, or treatment decisions, they may also require FDA clearance in the US or CE marking in the EU, meaning spending more resources on getting approvals.
How to handle compliance? Conduct an early regulatory assessment to define all frameworks at the start. Next, review your current systems and infrastructure: decide which systems must be connected, which ones replaced, and where data will be stored and processed.
Here are some extra points to consider:
- adopt a "compliance-by-design" architecture
- standardize APIs and data models
- strengthen data security and encryption standards
- establish a centralized compliance governance layer
- automate reporting and audit readiness
Note: Hiring experienced and certified software developers can help you complete integrations quickly and deploy solutions faster at a reasonable cost.
Security risks
725 data breaches affecting 500 or more records were detected in 2024 in the US only, and security has become the major concern when organizations decide to connect their proprietary, on-premises software with other systems.
The main directions here include ensuring data privacy and protecting patient records from cyber threats. HIPAA compliance remains a vital part of secure PHI storage, transmission, and processing for healthcare integrated solutions.
What you need to check:
- adherence to standards
- data encryption
- access controls
- secure data transmission and storage
- secure API connections
- data masking and anonymization
- audit trails and monitoring
When implementing integrations, ensure that they are as secure and compliant as the solutions themselves.
Lack of resources
For small hospitals and practices, innovation can be expensive and technically challenging. They might lack funds for overwhelming renovations, which include software and hardware updates, custom API development, extensive testing, staff training, and IT support, lagging behind market competition.
How to prepare for modernization? Detailed budget planning, feature prioritization, and step-by-step implementation might soften the burden. Have a clear strategy for integration, manage resistance to change, and plan staff training in advance.
Future trends in integrated healthcare solutions
There's no surprise that healthcare software integration will remain a trend itself. Yet, there are a lot of other tendencies that support data interoperability and are aimed at delivering patient-centered care and process optimization.
- Efficiency improvement. Over 70% of C-level executives report that efficiency improvement is the major priority for healthcare organizations in 2025, showing the enhanced adoption of connected data in the domain.
- Making healthcare more affordable. Healthcare costs remain one of the major challenges in the US — 3 in 10 respondents say they struggle to pay their current healthcare costs.
- AI integration in data processing. AI enhances healthcare by automating data mapping, standardising data, and detecting anomalies. It optimizes workflow processes and improves records quality and clinical decision-making.
- Increased investment in healthcare infrastructure modernization. With legacy systems being one of the major impediments to medical integration, the drive towards software and infrastructure updates will contribute to further interoperability advancements.
- Rise of IoMT use. The global IoMT market size is expected to grow at a CAGR of 26,09% between 2025 and 2034 and reach $2,294.87 billion by the end of the period. The Internet of Medical Things transfers health data without human interference, supporting the adoption of interconnected data in healthcare.
Conclusion
Healthcare technology integration can take different shapes and forms, yet one thing remains the same: the outspoken benefits of secure and smooth data exchange between all the participants.
While many challenges still hamper interoperability, we can see the increasing demand for interconnected systems. Both government and healthcare providers strive to meet patients' needs for secure, personalized treatment and affordable services.
Want to integrate data within your practice, clinic, or hospital? Contact NEKLO for a consultation on your project. With profound expertise in healthcare data standardization and adherence to regulatory compliance, we connect systems for smooth operations, reduced costs, and secure data flow.







.png)



